 March is National Colorectal Cancer Awareness Month and according to the National Institutes of Health (NIH), colorectal cancer – along with several other cancers such as esophagus, pancreas, breast, endometrium, kidney, thyroid and gallbladder – has been shown to have a significant association with obesity. A higher body mass index (BMI) is strongly associated with increased risk of colorectal cancer in men, and fat distribution seems to be an important factor, with abdominal obesity showing the strongest association. In women, there is also an association between BMI and colon cancer risk, but it is not as strong. One hypothesis about this relationship is that high levels of insulin or insulin-related growth factors in obese people may promote colon cancer development.
March is National Colorectal Cancer Awareness Month and according to the National Institutes of Health (NIH), colorectal cancer – along with several other cancers such as esophagus, pancreas, breast, endometrium, kidney, thyroid and gallbladder – has been shown to have a significant association with obesity. A higher body mass index (BMI) is strongly associated with increased risk of colorectal cancer in men, and fat distribution seems to be an important factor, with abdominal obesity showing the strongest association. In women, there is also an association between BMI and colon cancer risk, but it is not as strong. One hypothesis about this relationship is that high levels of insulin or insulin-related growth factors in obese people may promote colon cancer development.
According to the most recent annual report on cancer from the American Cancer Society, overall cancer rates are decreasing; however, incidence rates of some less common cancers have been increasing, including cancers of the pancreas, liver, thyroid and kidney. The reason for the increasing rates is unknown, but the report cites that obesity epidemic is probably associated with increases for some of these cancers. You can read more about the report here.
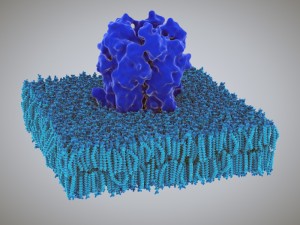
With obesity rates increasing, its association with colorectal and other cancers is particularly troubling, and research is focused on finding and addressing the mechanisms underlying obesity. This month, a study was published showing that defects in a protein that functions as a dietary fat sensor may be a cause of obesity and liver disease. The study was published in the journal Nature and the findings highlight a promising target for new drugs to treat obesity, as well as metabolic disorders. Researchers at the Imperial College London looked at the protein GPR120, which is found on the surface of cells in the gut, liver and fat tissue. GPR120 allows cells to detect and respond to unsaturated fatty acids, especially the omega-3 fatty acids which are believed to have a positive effect on health. They found that mice that are deficient in GPR120 were more likely to develop obesity and liver disease when given a high-fat diet. Additionally, people with a mutation in the gene encoding GPR120, which stops the protein from responding to omega-3 fatty acids, were significantly more likely to be obese. The study looked at GPR120 in nearly 7000 obese people and over 7600 controls to analyze whether differences in the genetic code that carries instructions for making the protein contribute to obesity. They found that one mutation that renders the protein dysfunctional increases a person’s risk of obesity by as much as 60%. The study authors explained that in both humans and mice, defects in GPR120 in combination with a high-fat diet, greatly increase the risk of collecting unhealthy fat around internal organs—a dangerous form of obesity. They concluded that GPR120 could be a useful target for new drugs to treat obesity and liver diseases.
Expert weight loss surgeon, Dr. Robert Snow of LoneStar Lap-Bands, commented on the article. He said “These new studies on colorectal cancer and the association with obesity are very important, since we know from prior studies, such as the Utah Study by Ted Adams and others, that cancer deaths and cardiovascular deaths were leading causes of premature death in morbidly obese patients who did not undergo bariatric surgery, compared to those who did.” Dr Snow concluded that the data shows again the association between BMI and incidence rates of colorectal cancer. This is very concerning when coupled with the lower rates of screening by colonoscopy, which was recently published in another study.
You can read more about the colonoscopy study here.






Weight Loss Studies & Clinical