 Obesity is a multifaceted disease that involves biological, behavioral, and environmental contributors. Energy imbalance is a primary component of the obesity problem, because weight gain results from consuming more calories than are burned. However, although many believe obesity can simply be solved by ‘eating less and moving more’ research is showing that the problem is much more complicated. A new study has shed light on how obesity and type 2 diabetes can create a stress response in the brain, especially in the hypothalamus. This is particularly important because the hypothalamus is the region of the brain that regulates appetite and energy production. This stress response may contribute to altering metabolism and creating an internal battle to control body weight.
Obesity is a multifaceted disease that involves biological, behavioral, and environmental contributors. Energy imbalance is a primary component of the obesity problem, because weight gain results from consuming more calories than are burned. However, although many believe obesity can simply be solved by ‘eating less and moving more’ research is showing that the problem is much more complicated. A new study has shed light on how obesity and type 2 diabetes can create a stress response in the brain, especially in the hypothalamus. This is particularly important because the hypothalamus is the region of the brain that regulates appetite and energy production. This stress response may contribute to altering metabolism and creating an internal battle to control body weight.
Researchers from the Joslin Diabetes Center studied the role of heat shock protein 60 (Hsp60) in hypothalamic insulin resistance and mitochondrial dysfunction in type 2 diabetes:
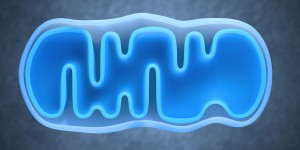
* Mitochondria are thought of as the “power plant” of the cell.
* Hsp60 is a stress response protein. It is supposed to protect mitochondria.
* Researchers observed that the level of Hsp60 decreases with obesity and type 2 diabetes.
* This decrease in levels of Hsp60 then decreases the efficiency of mitochondria.
* The decrease in the efficiency of mitochondria can lead to insulin resistance in the brain, and changes in metabolism.
“It’s a vicious cycle,” explained study senior author, C. Ronald Kahn, M.D. ” People become obese, then obesity disturbs the way the hypothalamus responds to stress, which makes people more likely to stay obese and become diabetic. The brain not only controls metabolism but the body’s metabolism affects the brain and aspects of brain function.” Are these negative effects permanent? The good news is that they do not seem to be, and they appear to have the potential to be reversed by weight loss. In addition, the findings may lead to the development of new drugs to boost Hsp60 levels and improve leptin sensitivity. The drug could potentially help obese people lose weight.
“There you go–we now know that the damage for the disease of obesity extends from your toes down to your tiny mitochondria!” said Dr. Tom Umbach, expert bariatric surgeon in Las Vegas. The findings are reported in the October issue of the Journal of Clinical Investigation.
Another recent study looked at the dynamics of mitochondria in the brain. Yale researchers studied mitochondria in different populations of brain cells known to be involved in the regulation of appetite. They found that during the transition from a fasting to an over-fed state, mitochondria in neurons that promote hunger show changes that are the opposite of those found in neurons that control feelings of fullness. You can read about that study here.
Related Reading: Brain’s Insulin Action Can Lead to Obesity






Weight Loss Studies & Clinical